Glaucoma
What Is Glaucoma?

Clear liquid called Aqueous Humor is constantly being produced within the eye. If the drainage angle of the eye is blocked, fluid cannot flow out of the eye.
Glaucoma is a disease of the optic nerve, which is part of the eye that carries the images we see to the brain. The optic nerve is made up of many nerve fibers, like an electric cable containing numerous wires. When pressure inside the eye increases, damage to the optic nerve fibers may occur, causing blind spots to develop. These blind spots usually go undetected until the optic nerve is significantly damaged. If the entire nerve is destroyed, blindness results.
Early detection and treatment are the keys to preventing optic nerve damage and blindness from glaucoma.
Glaucoma is a leading cause of blindness in the United States, especially for older people. But loss of sight from Glaucoma can be often be prevented with early detection and treatment.
What causes Glaucoma?
Clear liquid, called the aqueous humor, circulates inside the front portion of the eye. A small amount if this fluid is produced constantly, and an equal amount flows out of the eye through a microscopic drainage system, maintaining a constant level of pressure within the eye. (This liquid is not part of the tears on the outer surface of the eye.)
Because the eye is a closed structure, if the drainage area for the aqueous humor – called the drainage angle – is blocked, the excess fluid cannot flow out of the eye. Fluid pressure within the eye will increase, pushing against the optic nerve and potentially causing damage.
What are the different types of Glaucoma?
Chronic open-angle Glaucoma:
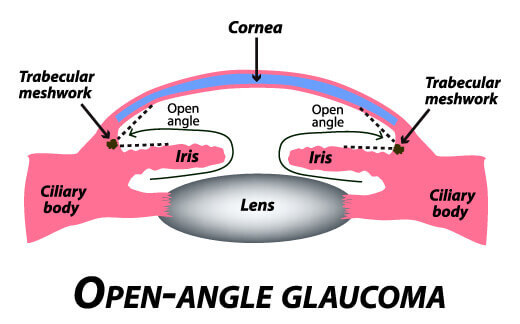
This is the most common form of glaucoma in the United States.
The risk of developing chronic open-angle glaucoma increases with age. The drainage angle of the eye becomes less efficient over time, and pressure within the eye gradually increases, which can damage the optic nerve. In some patients, the optic nerve becomes sensitive to normal eye pressure and is at risk for damage. Treatment is necessary to prevent further vision loss.
Chronic open-angle glaucoma damages vision so gradually and painlessly that you are not aware of trouble until the optic nerve is already injured.
Angle-closure Glaucoma:
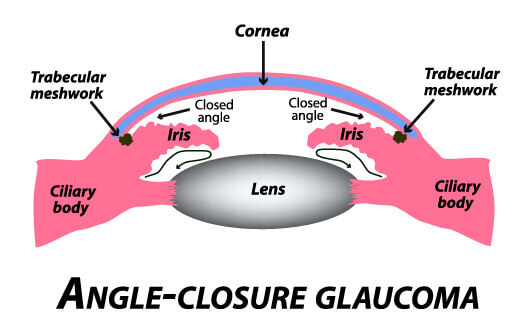
Sometimes the drainage angle of the eye may become completely blocked. In the eye, the iris (the part that makes eyes blue, brown or green) may drop over and completely close off the drainage angle. You can imagine this occurring much like a sheet if paper floating near a drain. If the paper suddenly drops over the opening, the flow is abruptly blocked.
When eye pressure builds up suddenly, an acute angle-closure glaucoma attack occurs.
Symptoms may include:
- Blurred vision
- Severe eye pain
- Headache
- Rainbow-colored halos around lights
- Nausea and vomiting
This is a true eye emergency. Unless this type of glaucoma is treated quickly, blindness can result.
In some patients, glaucoma has features of both the chronic open-angle type and the acute angle- closure type. This may be called chronic angle-closure glaucoma or mixed mechanism glaucoma.
Who is at risk for Glaucoma?
Many factors are considered to determine the risk for developing the disease.

The most important risk factors include:
- Age
- Family history of glaucoma
- African ancestry
- Past eye injuries
- All of these will be evaluated before deciding whether you need treatment for glaucoma, or whether you should be monitored closely as a glaucoma suspect. This means your risk of developing glaucoma is higher than normal, and you need to have regular examinations to detect the early signs of damage to the optic nerve.
How is Glaucoma detected?
Regular eye examinations are the best way to detect glaucoma. A glaucoma screening that checks only the pressure of the eye is not sufficient to determine if you have glaucoma. The only sure way to detect glaucoma is to have a complete eye examination.
During your glaucoma evaluation, Dr. Paveloff will:
- Measure your intraocular pressure (tonometry)
- Inspect the drainage angle of your eye (gonioscopy)
- Evaluate whether or not there is any optic nerve damage (ophthalmoscopy)
- Test the peripheral vision of each eye (visual field testing or perimetry.)
- Optic Nerve Head analysis via HRT/GDX imaging Photography of the optic nerve or other computerized imaging may be recommended. Some of these tests may need to be repeated on a regular basis to monitor any changes in your condition.
How is Glaucoma treated?
As a rule, damage caused by glaucoma cannot be reversed. Eye drops, laser surgery and surgery in the operating room are methods used to help prevent further damage. In some cases, oral medications may also be prescribed.
With any type of glaucoma, periodic examinations are very important to prevent vision loss. Because glaucoma can progress without your knowledge, adjustments to your treatment may be necessary from time to time.
Medications
Glaucoma is usually controlled with eye drops taken on a daily basis. These medications decrease eye pressure, either by slowing the amount of aqueous fluid produced within the eye or by improving the flow through the drainage angle.
Glaucoma medications can preserve your vision, however, they may also produce side effects. You should notify your ophthalmologist if you think you may be experiencing side effects.

Some eye drops may cause:
- A stinging sensation
- Red eyes or redness of the skin surrounding the eyes
- Changes in pulse or heartbeat
- Changes in breathing (especially with asthma or emphysema)
- Dry mouth
- Changes in sense of taste
- Headaches
- Blurred vision
- All medication can have side effects or can interact with other medications. Therefore, it is important that you make a list of the medications you regularly take and share this list with each doctor you see.
Selective Laser Trabeculoplasty (SLT)
Laser surgery treatments may be recommended for different types of glaucoma. In open-angle glaucoma, the drain itself is treated. The laser is used to modify the drain (trabeculoplasty) to help control eye pressure.
In angle-closure glaucoma, the SLT laser creates a hole in the iris (iridotomy) to improve the flow of aqueous fluid to the drain.
Surgery
When surgery is needed to treat glaucoma, Dr. Paveloff uses fine, microsurgical instruments to create a new drainage channel for the aqueous fluid to leave the eye. Should this type of surgery be necessary, we can provide you with information about his procedure. As with laser surgery, this is typically an outpatient procedure.
There are risks with all types of surgery. Though serious complications of modern glaucoma surgery are uncommon, they can occur. Surgery is recommended if it is necessary to prevent further damage to the optic nerve.
MIGS – Minimally Invasive Glaucoma Surgery

In general, the goal of all types of glaucoma surgery is to lower eye pressure to prevent or reduce damage to the optic nerve. MIGS has been specifically developed with the goal of reducing the risk of complications associated with more traditional glaucoma surgeries.
MIGS includes a group of procedures that use microscopic-sized equipment and minimal incisions in the eye. These procedures can be highly effective for treating mild to moderate cases of glaucoma. Types of MIGS procedures are:
- Microtrabeculectomies. Microscopic-sized tubes are inserted into the eye to drain fluid. These devices are excellent at lowering pressure in the eye and safer than traditional trabeculectomy devices.
- Trabecular surgery. Through a special contact lens on the eye, a tiny device is inserted via a small incision into the trabecular meshwork. The damaged meshwork can then be destroyed or bypassed. This is most effective for early to moderate stages of glaucoma. The OMNI, HYDRUS and iStent devices can lower intraocular eye pressure as much as 30-40%.
- Suprachoroidal shunts. Small tubes are inserted to connect the front of the eye to the suprachoroidal space in order to support fluid draining from the eye. This procedure is effective at lowering eye pressure in moderately severe cases of glaucoma and has an extremely low rate of complications.
- Milder versions of laser photocoagulation. Recent advances in the laser treatment of glaucoma include endocyclophotocoagulation and micropulse cyclophotocoagulation. These procedures help to reduce the eye’s ability to produce fluid and can assist with advanced stages of glaucoma.
What is your part in treatment?
Treatment for glaucoma requires teamwork between you and your doctor. Dr. Paveloff can prescribe treatment for glaucoma, but only you can make sure that you follow instructions and take your eye drops.
Once you are taking medication for glaucoma, Dr. Paveloff will want to see you more frequently. Typically, you can expect to be seen every three to four months. This will vary depending on your treatment needs.
Loss of vision can be prevented
Regular medical eye exams may help prevent unnecessary vision loss.
Recommended intervals for eye exams are:
- Age 20-39: individuals of African descent or with family history of glaucoma should have a medical exam every 3 to 5 years. Others can be seen at least once during this period.
- Age 40-64; Every 2 to 4 years
- Age 65 or older; Every 1 to 2 years
Paveloff Vision Center offers a wide range of financing options. Click here to learn more!

